You, Your Diet and Your Microbiome
The relationship between our health, our dietary choices, and our gut microbiome is a fascinating research topic. We are only starting to understand the deep connection between the microbiome and our health. Read on for an overview of what the current scientific literature is beginning to unfold about this symbiotic relationship.
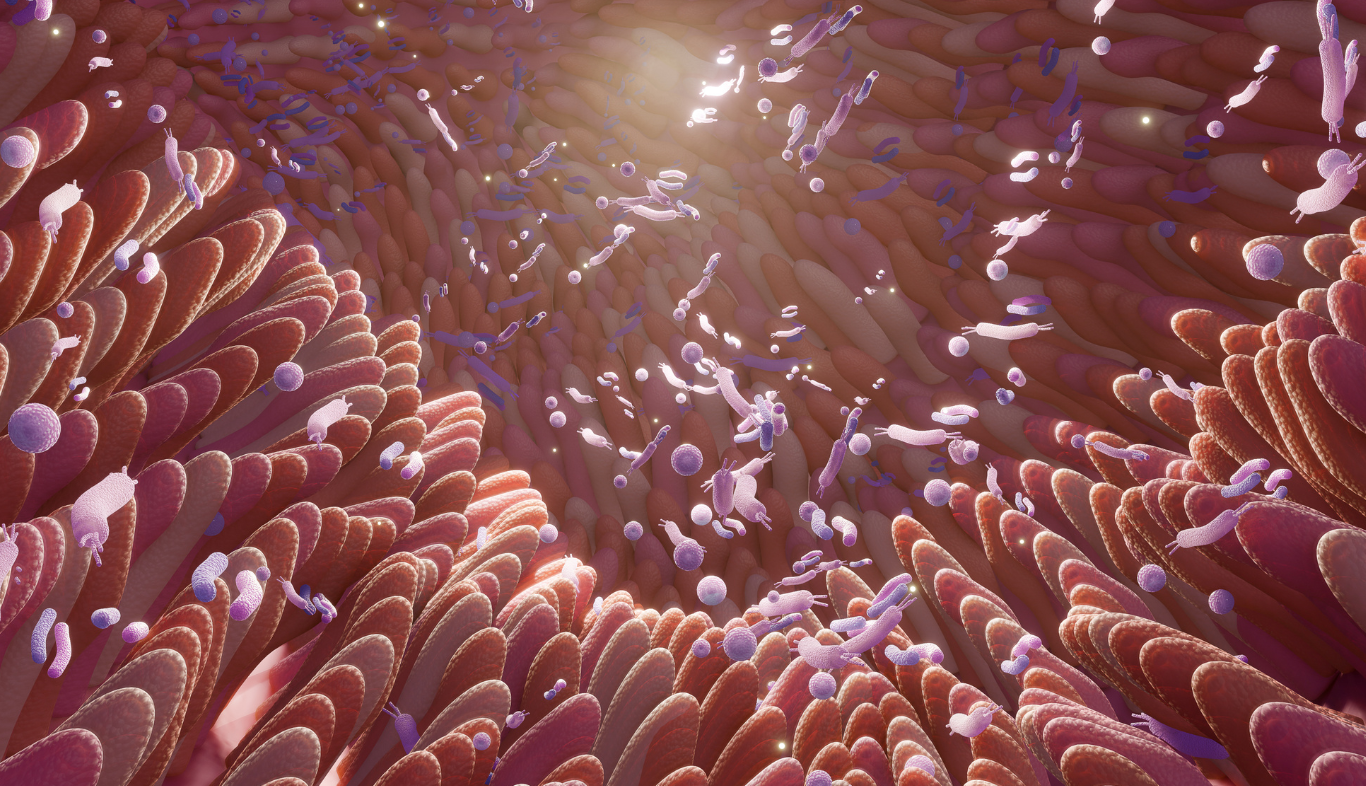
What is the microbiome?
The relationship between our microbiome and us
We are only starting to understand the deep connection between the microbiome and our health. Throughout human evolution, we have cooperated with microorganisms, borrowing their genes as evolutionary shortcuts to acquire new capabilities (3).
In the large intestine, microorganisms synthesise a multitude of metabolites impacting our metabolism, and influencing how nutrients are stored and processed by the liver and muscle cells. For example, these molecules can determine whether glucose should be stored as fat or glycogen and affect the response to insulin (4). These are only some interesting facts about the microbiota, and as scientific research advances, we are starting to understand more about it.
How do the bacteria in our gut communicate with the brain?
Our gut bacteria communicate with the brain through neural, endocrine, and immune signalling mechanisms. The brain uses the autonomic nervous system to regulate gut movements, secretions, permeability, and hormone secretions; these can directly affect the microbiome and its gene expression (5). This bidirectional system is known as the gut-brain axis. Changes in the brain-gut-microbiome communication appear to be involved in the pathophysiology of conditions such as irritable bowel syndrome (6). Bacterial compounds can even regulate appetite and weight and influence hormones and neurotransmitters, thus controlling our mood, energy levels and behaviour (7, 8).
How our dietary choices can positively impact our microbiome
Research shows that nutrition appears to be one of the most important factors impacting the composition of our microbiome (9). Long-term dietary changes, particularly the consumption of fibre from fruits, vegetables, and grains, have been linked to an increased prevalence of microbes associated with a healthy gut (11, 12). These health-promoting bacteria can ferment dietary fibre into short-chain fatty acids (SCFA) (13). This fermentation process leads to a decrease in colon pH (14). The lowered pH inhibits the growth of acid-sensitive and harmful bacteria and promotes the growth of beneficial types of bacteria such as Firmicutes (14). Ongoing research on SCFA is exploring their health effects, including their ability to modulate inflammation, maintain normal blood glucose and cholesterol levels and stimulate immune cell activity (15, 16). They play a crucial role in gut health as they provide energy for enteric bacteria and help prevent excessive cell growth, promoting apoptosis and cell differentiation and might help prevent colon cancer (17-19). SCFAs can also directly impact metabolism, regulating factors like body weight and diabetes through epigenetic mechanisms (18).
The microbiota of the African children was high in Bacteroidetes and low in Firmicutes. Moreover, the African children’s microbiota was abundant in bacteria specialised in breaking down cellulose and xylan (two types of dietary fibre). Additionally, in the African children, the presence of Enterobacteriaceae such as Shigella and Escherichia (i.e. two potentially pathogenic groups of bacteria) was considerably lower. This observation has led to the hypothesis that the gut microbiota of African children coevolved in response to Western African diets high in polysaccharides and dietary fibre. This particular type of microbiota maximises energy production from dietary fibre, and it might provide protection against inflammation and non-infectious intestinal diseases (20).

Dietary fibre, microbiome and inflammation
However, a more recent trial showed that in people with poor microbiome diversity, a sudden increase in dietary fibre increased SCFA but also inflammatory markers (25). The study also involved another arm which involved the administration of fermented foods such as yoghurt, kombucha and kimchi. In this group, the inflammation markers decreased while the microbiome diversity increased. The study results suggested that a gradual increase in both dietary fibre and fermented foods might be an ideal strategy to slowly improve microbiome diversity, reduce inflammation and increase the production of health-promoting metabolites such as SCFA (25).

Plant-based diets, omnivore diets and their effects on the microbiome
Animal-based foods can provide specific nutrients that may be involved in cardiovascular health. For example, certain animal-based foods contain choline and carnitine, which can be metabolised by specific bacteria into compounds like trimethylamine N-oxide (TMAO). TMAO has been linked with adverse cardiovascular outcomes (27, 28). However, it is not clear yet if TMAO is a mediator or a bystander in the disease process and more research is needed in this area (29).
Regardless of whether one follows a plant-based or omnivorous diet, what matters most for promoting a healthy microbiota is consuming a diet high in vegetables, whole grains, legumes, fruit and nuts. These foods are high in dietary fibre which is the favourite food of our microbiome! The Mediterranean diet is a good example of a healthy plant-based dietary pattern.
The bottom line
The microbiome can be considered one of the most important links between our diet and our health. The current literature shows a symbiotic communication between our body and our microbiome, whose details aren’t fully understood yet. This makes the microbiome one of the most exciting and cross-cutting research topics. Eating a diet full of tasty whole plant-based foods is an ideal strategy to grow and maintain a healthy microbiome.
Further information
The PAN website hosts a large collection of webinar recordings on various nutrition and health topics, including a number of expert lectures on the gut microbiome. The webinars are available to PAN Members along with many other valuable educational resources. Find out more about how to access these webinars here: https://pan-int.org/webinar-recordings/
Webinars in English
- Effects of Nutrition on the Gut Microbiome and Metabolic Health by Emanuel Canfora, Ph.D.
- Diet and Diabetes: Carbohydrate Consensus vs. Controversy by Christopher Gardner, Ph.D.
- Vegan nutrition and irritable bowel syndrome by Prof. Büning & Amelie Kahl
- The effect of the Mediterranean Diet on the gut microbiome (Journal Club) by Dr Conrad Shultz-Ruhtenberg
Webinars in German
- The importance of the microbiome in the development and therapy of diseases by Jun.-Prof. Marie-Christine Simon, PhD, RD
- Nutrition in the Prevention and Therapy of Autoimmune Diseases & Fasting in Medicine by Prof. Dr. Andreas Michalsen
- Diagnostics and therapy for IBS, leaky gut syndrome by Prof. Dr. med. Stephan C. Bischoff
- What is the microbiome? By Dr. Philipp Busche, Anna-Maria Bramböck and Prof. Dr. med. Dr. phil. Lia Bally

Making better physicians
Ready to improve your nutrition knowledge?
Sign up for the PAN Academy and take our free online courses on nutrition science.
Mini Modules on Diet-Related Diseases
This series of short modules addresses common diet-related diseases such as heart disease, hypertension and type 2 diabetes. Learn the causes and which patients are at risk, and find out practical solutions to managing these diseases through whole food, plant-based eating.



Making better physicians
Ready to improve your nutrition knowledge?
Sign up to the PAN Academy and take our free online courses on nutrition science.
Mini Modules on Diet-Related Diseases
This series of short modules addresses common diet-related diseases such as heart disease, hypertension and type 2 diabetes. Learn the causes and which patients are at risk, and find out practical solutions to managing these diseases through whole food, plant-based eating.
References List:
- Valdes AM, Walter J, Segal E, Spector TD. Role of the gut microbiota in nutrition and health. The BMJ. 2018 Jun 13;361:k2179.
- International Human Genome Sequencing Consortium. Finishing the euchromatic sequence of the human genome. Nature. 2004 Oct 21;431(7011):931–45.
- Bäckhed F, Ley RE, Sonnenburg JL, Peterson DA, Gordon JI. Host-Bacterial Mutualism in the Human Intestine. Science. 2005 Mar 25;307(5717):1915–20.
- Wu J, Wang K, Wang X, Pang Y, Jiang C. The role of the gut microbiome and its metabolites in metabolic diseases. Protein Cell. 2021 May;12(5):360–73.
- Martin CR, Osadchiy V, Kalani A, Mayer EA. The Brain-Gut-Microbiome Axis. Cell Mol Gastroenterol Hepatol. 2018 Apr 12;6(2):133–48.
- Labus JS, Hollister EB, Jacobs J, Kirbach K, Oezguen N, Gupta A, et al. Differences in gut microbial composition correlate with regional brain volumes in irritable bowel syndrome. Microbiome. 2017 May 1;5(1):49.
- van de Wouw M, Schellekens H, Dinan TG, Cryan JF. Microbiota-Gut-Brain Axis: Modulator of Host Metabolism and Appetite. J Nutr. 2017 May;147(5):727–45.
- Sasso JM, Ammar RM, Tenchov R, Lemmel S, Kelber O, Grieswelle M, et al. Gut Microbiome–Brain Alliance: A Landscape View into Mental and Gastrointestinal Health and Disorders. ACS Chem Neurosci. 2023 May 8;14(10):1717–63.
- Rothschild D, Weissbrod O, Barkan E, Kurilshikov A, Korem T, Zeevi D, et al. Environment dominates over host genetics in shaping human gut microbiota. Nature. 2018 Mar;555(7695):210–5.
- Jardon KM, Canfora EE, Goossens GH, Blaak EE. Dietary macronutrients and the gut microbiome: a precision nutrition approach to improve cardiometabolic health. Gut. 2022 Jun 1;71(6):1214–26.
- De Filippis F, Pellegrini N, Vannini L, Jeffery IB, La Storia A, Laghi L, et al. High-level adherence to a Mediterranean diet beneficially impacts the gut microbiota and associated metabolome. Gut. 2016 Nov;65(11):1812–21.
- Sonnenburg ED, Smits SA, Tikhonov M, Higginbottom SK, Wingreen NS, Sonnenburg JL. Diet-induced extinctions in the gut microbiota compound over generations. Nature. 2016 Jan 14;529(7585):212–5.
- Kang J, Yin S, Liu J, Li C, Wang N, Sun J, et al. Fermentation models of dietary fibre in vitro and in vivo – A review. Food Hydrocoll. 2022 Oct 1;131:107685.
- Holscher HD. Dietary fiber and prebiotics and the gastrointestinal microbiota. Gut Microbes. 2017 Mar 4;8(2):172–84.
- He J, Zhang P, Shen L, Niu L, Tan Y, Chen L, et al. Short-Chain Fatty Acids and Their Association with Signalling Pathways in Inflammation, Glucose and Lipid Metabolism. Int J Mol Sci. 2020 Sep 2;21(17):6356.
- Corrêa-Oliveira R, Fachi JL, Vieira A, Sato FT, Vinolo MAR. Regulation of immune cell function by short-chain fatty acids. Clin Transl Immunol. 2016 Apr 22;5(4):e73.
- Hinnebusch BF, Meng S, Wu JT, Archer SY, Hodin RA. The effects of short-chain fatty acids on human colon cancer cell phenotype are associated with histone hyperacetylation. J Nutr. 2002 May;132(5):1012–7.
- Remely M, Aumueller E, Merold C, Dworzak S, Hippe B, Zanner J, et al. Effects of short chain fatty acid producing bacteria on epigenetic regulation of FFAR3 in type 2 diabetes and obesity. Gene. 2014 Mar 1;537(1):85–92.
- Mirzaei R, Afaghi A, Babakhani S, Sohrabi MR, Hosseini-Fard SR, Babolhavaeji K, et al. Role of microbiota-derived short-chain fatty acids in cancer development and prevention. Biomed Pharmacother. 2021 Jul 1;139:111619.
- De Filippo C, Cavalieri D, Di Paola M, Ramazzotti M, Poullet JB, Massart S, et al. Impact of diet in shaping gut microbiota revealed by a comparative study in children from Europe and rural Africa. Proc Natl Acad Sci U S A. 2010 Aug 17;107(33):14691–6.
- Bäckhed F, Fraser CM, Ringel Y, Sanders ME, Sartor RB, Sherman PM, et al. Defining a healthy human gut microbiome: current concepts, future directions, and clinical applications. Cell Host Microbe. 2012 Nov 15;12(5):611–22.
- Cordonnier C, Le Bihan G, Emond-Rheault JG, Garrivier A, Harel J, Jubelin G. Vitamin B12 Uptake by the Gut Commensal Bacteria Bacteroides thetaiotaomicron Limits the Production of Shiga Toxin by Enterohemorrhagic Escherichia coli. Toxins. 2016 Jan 5;8(1):14.
- Wagenaar CA, van de Put M, Bisschops M, Walrabenstein W, de Jonge CS, Herrema H, et al. The Effect of Dietary Interventions on Chronic Inflammatory Diseases in Relation to the Microbiome: A Systematic Review. Nutrients. 2021 Sep 15;13(9):3208.
- IDF Diabetes Atlas 2021 | IDF Diabetes Atlas [Internet]. [cited 2023 Mar 6]. Available from: https://diabetesatlas.org/atlas/tenth-edition/
- Wastyk HC, Fragiadakis GK, Perelman D, Dahan D, Merrill BD, Yu FB, et al. Gut-microbiota-targeted diets modulate human immune status. Cell. 2021 Aug 5;184(16):4137-4153.e14.
- Tomova A, Bukovsky I, Rembert E, Yonas W, Alwarith J, Barnard ND, et al. The Effects of Vegetarian and Vegan Diets on Gut Microbiota. Front Nutr [Internet]. 2019 [cited 2023 Mar 16];6. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6478664/
- Fretts AM, Hazen SL, Jensen P, Budoff M, Sitlani CM, Wang M, et al. Association of Trimethylamine N-Oxide and Metabolites With Mortality in Older Adults. JAMA Netw Open. 2022 May 20;5(5):e2213242.
- Yang S, Li X, Yang F, Zhao R, Pan X, Liang J, et al. Gut Microbiota-Dependent Marker TMAO in Promoting Cardiovascular Disease: Inflammation Mechanism, Clinical Prognostic, and Potential as a Therapeutic Target. Front Pharmacol [Internet]. 2019 [cited 2023 Mar 6];10. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6877687/
- Velasquez MT, Ramezani A, Manal A, Raj DS. Trimethylamine N-Oxide: The Good, the Bad and the Unknown. Toxins. 2016 Nov 8;8(11):326.
Recent posts
Alzheimer’s Disease: Decode the Complex Puzzle
Alzheimer’s is a complex puzzle. Learn about genetic factors and how recommending a whole food, plant-based diet can elevate patient care.
A Patient Guide to Outsmarting Alzheimer’s Disease
Learn how dietary choices impact Alzheimer’s risk. Discover measures that can slow progression and reduce its effects.
Easy Plant-Based Swaps
Make your transition to a whole food, plant-based diet stick. Explore delicious and easy plant-based swaps to add more plants to your plate.
Manage Your Rheumatoid Arthritis With Diet
Manage rheumatoid arthritis naturally with a plant-based diet. Reduce inflammation, ease joint pain, and improve your overall health.
Rheumatoid Arthritis and Diet: A Physician’s Guide
Rheumatoid Arthritis and Diet: A Physician’s GuideBy Carlijn Wagenaar, MD and Wendy Walrabenstein, RD from PAN The...
Heart Disease: A Patient Guide to Prevention and Reversal
Discover how to prevent and reverse heart disease. Learn about the advantages of lifestyle changes with a whole food plant-based diet.
Heart Disease Uncovered: A Physician’s Guide
Uncover the secrets to prevent and reverse heart disease. Learn how a whole food plant-based diet can help patients lead a heart-healthy life.
Treating the Silent Killer: Hypertension Insights and Solutions
Explore the power of plant-based diets in managing hypertension. Empower your patients to take control of their blood pressure readings.
Hypertension: A Patient Guide to Reducing High Blood Pressure
Is high blood pressure dangerous? What can you do to manage hypertension and reduce your risk of other related diseases?
Carbohydrates: A Complex or Simple Matter?
Are carbohydrates essential for our health? Do low-carb diets yield greater weight loss? What benefits do whole plant-based foods provide? Find out the answers to these questions and more in this blog post.