Uncovering the Truth About Your Diet: Objective Strategies for Dietary Assessment
By Dr. Miriam Sonntag from the PAN Academy – our online learning platform where you can learn all about nutrition science. Do you want to know more about this topic? Check out Module 3 “Evaluation of Nutrition Studies” where we go into many more details about how to navigate the world of science literature.
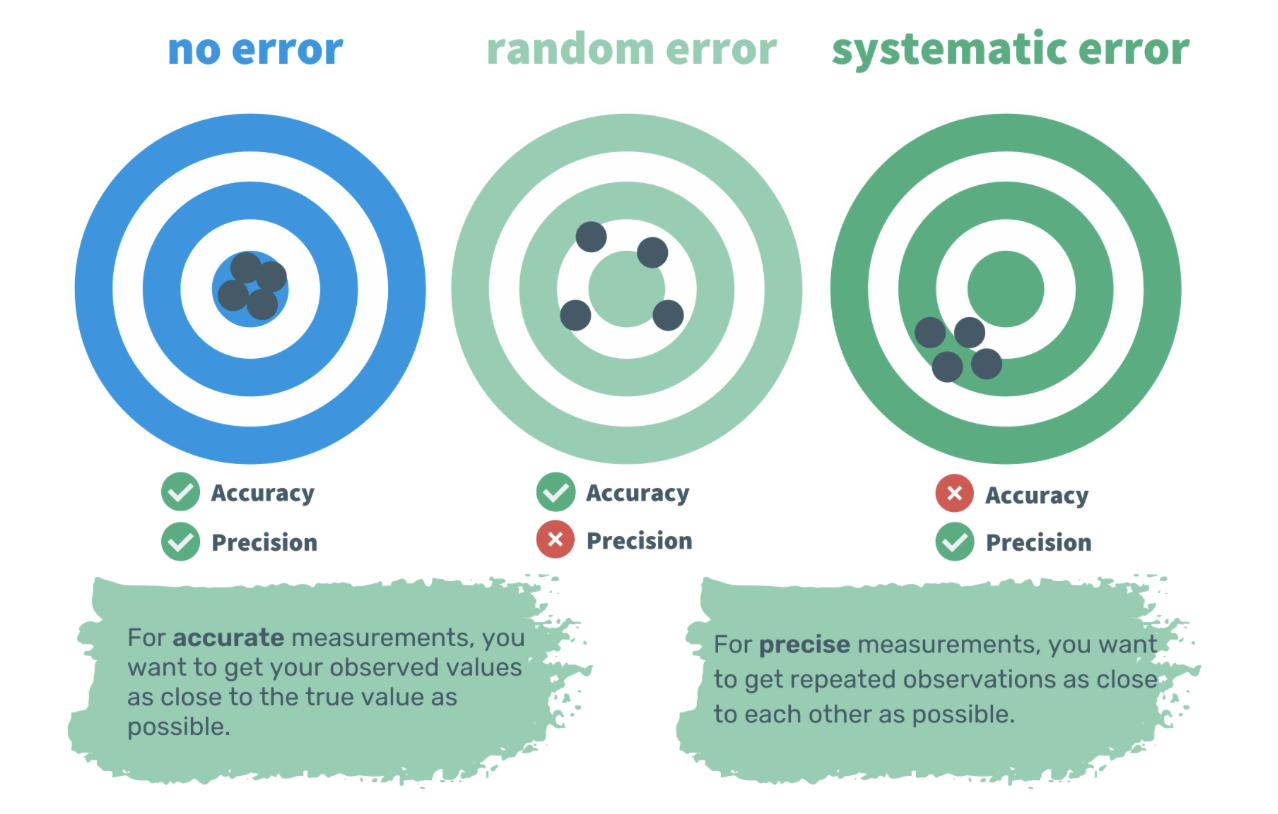
What we eat matters! But how do we know what people are really eating? Most nutrition studies rely on dietary assessment methods such as food frequency questionnaires (FFQs), 24-hour recalls, and food diaries. All these methods depend on people reporting what they eat. But obtaining accurate data is not easy. Misreporting food intake is a big problem. In this article, we will explore how people misreport and how to improve the accuracy of dietary data.
Problem #1 – Estimating the Correct Portion Size
One reason for inaccurate reporting is estimating the correct portion size. Ideally, the most accurate method would be to weigh and keep track of every food item in real time. Not only the serving size, but also any leftovers, should be recorded in a food diary.
Weighed food diaries are the gold standard method for dietary assessment in clinical trials. Yet, tracking every sip and bite in real time for more than 3 – 4 days in a row is burdensome and time-consuming. That is why retrospective methods like 24-hour-recalls or Food Frequency Questionnaires (FFQs) are more common (1).
Although frequently used, retrospective methods rely on our memory. This can be problematic as our memory is prone to forgetting key details like the type and quantity of food consumed. Foods and drinks habitually consumed might be easier to recall. But what about seasonal foods and foods consumed not so often? The recorded intakes may be less accurate. Moreover, small, medium, and large are not standard measures everywhere in the world. For example, in Italy a small cappuccino is around 150 ml, whereas in the US a small cappuccino is around 360 ml.
The more accurate the estimation of portion size, the better the dietary analysis. But how do we achieve more accuracy? Weighing foods is too cumbersome and using small, medium, and large measurements is too imprecise. A better approach would be to use image-assisted methods (2).
Solution #1 – Image-Assisted Dietary Assessment Methods
As the name implies, image-assisted methods rely on food images. Not long ago, dieticians used a food atlas which included pictures of the same food or dish but in different portion sizes. Today, these methods are built into smartphone apps. The advantage of these apps is that they can estimate the quantity and quality of foods consumed, and any leftovers, through a smartphone camera. The food images are then sent to clinicians or researchers for analysis in real-time.
To further reduce the burden of analysis, fully automated image-based approaches have been developed. The captured food images are sent to a central server for analysis. Instead of a trained human being, software compares the captured food images with images in the database (3). These methods are still in their infancy and need further testing and validation.
The image-assisted and image-based methods offer an improvement in the accuracy of portion size estimation. Yet, they are not perfect. Apps can remind users, but they cannot ensure that all food and drinks are captured throughout the day. Therefore, even if accuracy is improved, the reporting might still be incomplete.
Problem #2 – Unintentional and Intentional Misreporting
To understand the drivers of chronic diseases, we need to look at what people usually eat. What are their eating patterns over years or even decades? To identify eating patterns, we need to capture three to seven days, including one weekend day.
Studies have indicated that the more days captured, the higher the burden and likelihood of misreporting (4). Single food items like snacks, calorie-containing beverages or even whole meals might be forgotten. Unhealthy foods, high in fat or sugar, might be underreported. Whereas, healthy foods, like fresh fruits and vegetables, might be overreported.
Other factors, including body image, body weight, age, and gender can also affect how accurately people report their food intake (5). For example, studies have indicated that women tend to underreport more often than men (6). Greater underreporting has been observed in overweight or obese individuals, exhibiting a social desirability bias (7). In these cases, underreporting food or drink intake may be a way to avoid criticism and adhere to perceived social norms.
Furthermore, people might change their eating habits while reporting. Why? Because they aim to simplify the reporting process or become more mindful when preparing and eating foods. This effect is known as the observer effect or reactivity. Once the reporting phase has ended, these new habits may not be maintained, rendering the reported information unreliable.
Solution #2 – Wearable Devices
One way to overcome this issue are wearable devices that automatically take pictures every couple of seconds (2). They reduce the burden of capturing everything we eat and drink throughout the day. They can record a more detailed picture of what, how much, when and where we eat. Yet, the more pictures are captured, the more time is needed to review them.
Wearable devices are also in their infancy and need further testing and evaluation. But as technology advances, new tools might emerge. There might be swallowable cameras or hand-to-mouth movement trackers in the future. Let’s keep an eye on promising technological advancements!
Meanwhile, there are other options to improve the reporting of food intake. We can use a more integrated approach. We can complement self-report techniques with nutritional biomarkers, for example (8,9).
An Integrated Approach
Nutritional biomarkers can provide a more objective measurement of what and how much has been consumed. Examples of well-validated biomarkers include urinary nitrogen for protein, serum carotenoids for vegetables and fruits, and omega-3 fatty acids for oily fish. Currently, the list of biomarkers for nutrient intake is short. But it will grow as analytical chemistry advances.
It is possible to measure thousands of metabolites simultaneously, and in different samples, including erythrocytes, urine, serum, salvia, and hair. These new techniques not only allow the identification of new metabolites, but can provide new insights into the complex diet-disease interactions (10).
Recent studies have identified multi-metabolite profiles related to specific diets like the Mediterranean and Western diet. These profiles can then be used to unravel why and how a healthy plant-based diet can lower the risk of type 2 diabetes, for example (11). Additionally, we could use these profiles to assess how strictly people adhere to a specific diet.
With advances in technology and methods, dietary assessment is becoming easier and better. New methods are unlikely to replace traditional methods such as food diaries. But we can combine them to get a better picture of what and how much people consume. Evidence shows that nutritional biomarkers might be more sensitive, robust and specific (12). They can be used to confirm if the reported intake levels are plausible or identify dietary patterns. Even in blood samples never meant for assessing diets.
Additional Information:
-
Dr Miriam Sonntag is the Medical Content Executive of the online learning platform, PAN Academy. Having worked in basic research, she knows how to decipher complex information. Working now at PAN, she scans and pours over scientific papers and books. She breaks down the latest nutritional research into actionable advice for everyday life. She is committed to sharing the bigger picture of why it is good to put more plants on your plate.
-
Are you interested in how many metabolites have been identified already? Then check out the FoodDB. You can browse either foods or compounds.
-
Dao MC, Subar AF, Warthon-Medina M, Cade J, Burrows T, Golley RK, et al. Dietary Assessment Toolkits: An Overview. Public Health Nutr. 2019 Mar;22(3):404–18.
Höchsmann C, Martin CK. Review of the validity and feasibility of image-assisted methods for dietary assessment. Int J Obes 2005. 2020 Dec;44(12):2358–71.
Boushey CJ, Spoden M, Zhu FM, Delp EJ, Kerr DA. New mobile methods for dietary assessment: review of image-assisted and image-based dietary assessment methods. Proc Nutr Soc. 2017 Aug;76(3):283–94.
Whybrow S, Horgan GW, Macdiarmid JI. Self-reported food intake decreases over recording period in the National Diet and Nutrition Survey. Br J Nutr. 2020 Sep;124(6):586–90.
Miller TM, Abdel-Maksoud MF, Crane LA, Marcus AC, Byers TE. Effects of social approval bias on self-reported fruit and vegetable consumption: a randomized controlled trial. Nutr J. 2008 Jun 27;7:18.
Horner NK, Patterson RE, Neuhouser ML, Lampe JW, Beresford SA, Prentice RL. Participant characteristics associated with errors in self-reported energy intake from the Women’s Health Initiative food-frequency questionnaire1,2,3. Am J Clin Nutr. 2002 Oct 1;76(4):766–73.
Harrison GG, Galal OM, Stormer A, Leslie J, Ibrahim N, Khorshid A, et al. Underreporting of Food Intake by Dietary Recall Is Not Universal: A Comparison of Data from Egyptian and American Women. J Nutr. 2000 Aug 1;130(8):2049–54.
Castellano-Escuder P, González-Domínguez R, Vaillant MF, Casas-Agustench P, Hidalgo-Liberona N, Estanyol-Torres N, et al. Assessing Adherence to Healthy Dietary Habits Through the Urinary Food Metabolome: Results From a European Two-Center Study. Front Nutr. 2022;9:880770.
Schulz CA, Oluwagbemigun K, Nöthlings U. Advances in dietary pattern analysis in nutritional epidemiology. Eur J Nutr. 2021 Dec;60(8):4115–30.
Brouwer-Brolsma EM, Brennan L, Drevon CA, van Kranen H, Manach C, Dragsted LO, et al. Combining traditional dietary assessment methods with novel metabolomics techniques: present efforts by the Food Biomarker Alliance. Proc Nutr Soc. 2017 Nov;76(4):619–27.
Wang F, Baden M, Guasch-Ferré M, Wittenbecher C, J L, Y L, et al. Plasma metabolite profiles related to plant-based diets and the risk of type 2 diabetes. Diabetologia [Internet]. 2022 Jul [cited 2023 Mar 30];65(7). Available from: https://pubmed.ncbi.nlm.nih.gov/35391539/
Playdon MC, Moore SC, Derkach A, Reedy J, Subar AF, Sampson JN, et al. Identifying biomarkers of dietary patterns by using metabolomics. Am J Clin Nutr. 2017 Feb;105(2):450–65.