Treating the Silent Killer: Hypertension Insights and Solutions
By Dr. Miriam Sonntag from the PAN Academy – our online learning platform where you can learn all about nutrition and health.
High blood pressure, or hypertension, affects over 1.4 billion people worldwide. That’s roughly 1 in 4 men and 1 in 5 women. Alarmingly, an estimated 700 million individuals remain unaware (1). This silent threat claims nine million lives each year and heightens the risk of heart disease and stroke (2). This blog post explores the relationship between salt and hypertension. Moreover, it will uncover the efficacy of plant-based diets in prevention and treatment.
Healthy blood pressure
Before delving into the mechanisms of hypertension, let’s revisit blood pressure fundamentals. European and American guidelines indicate optimal blood pressure below 120/80 mmHg (3). The top number indicates systolic pressure during heart contraction, and the bottom number represents the diastolic pressure between heartbeats.
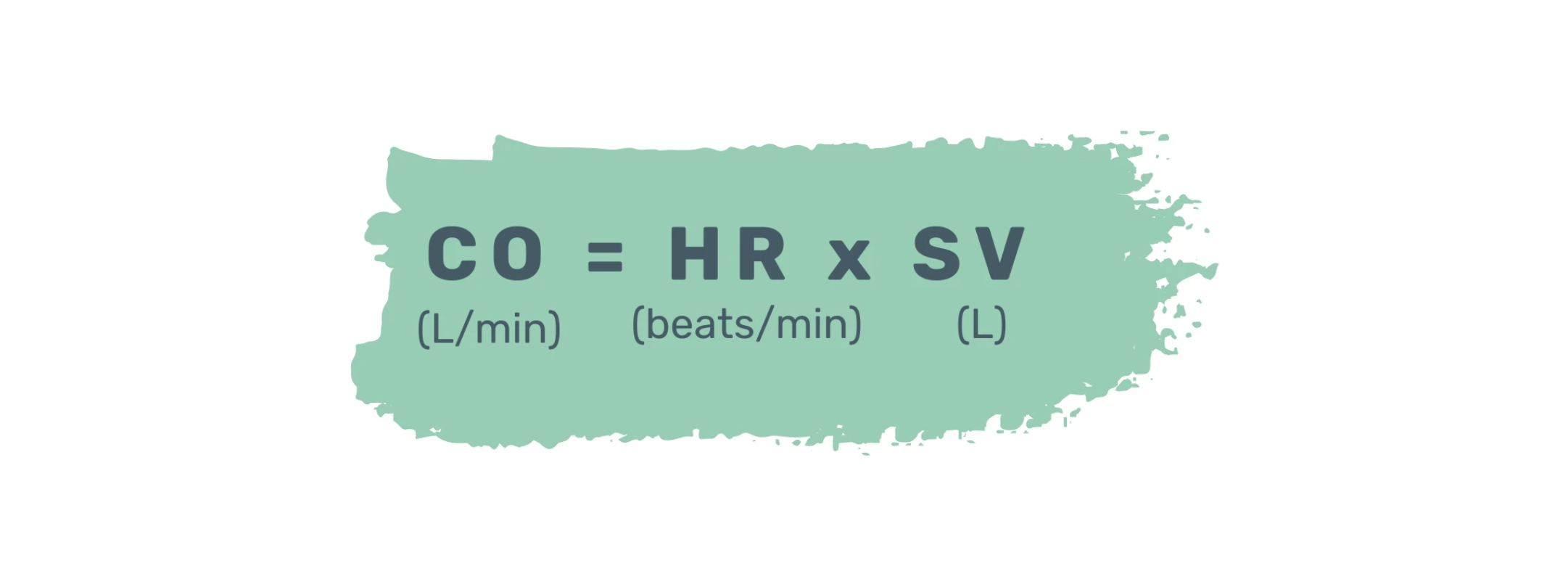
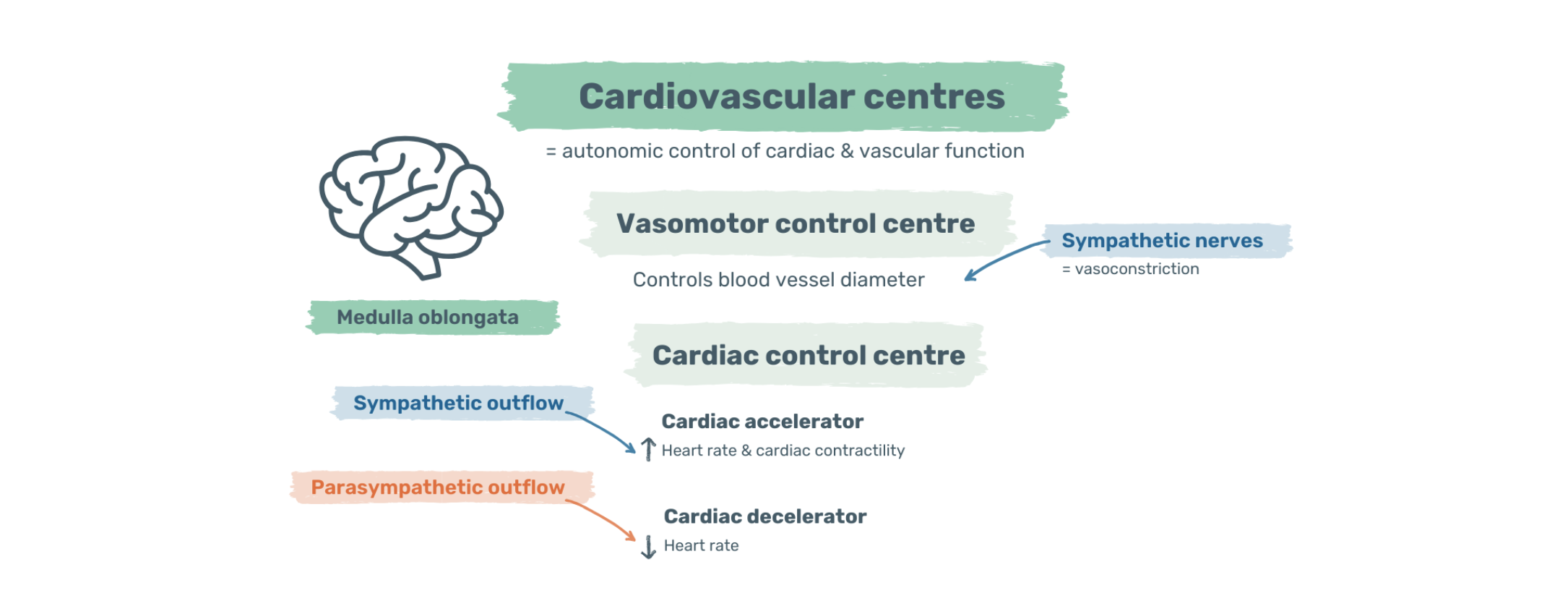
Blood pressure relies on two key factors controlled by the autonomic nervous system: cardiac output and vascular resistance. Cardiac output, governed by heart rate and stroke volume, affects the blood volume ejected per minute. Sympathetic nerves increase heart rate, raising pressure, while parasympathetic nerves counter this effect.
Image: Cardiac output measures the amount of blood the heart pumps in one minute. To calculate it, multiply the heart rate by the stroke volume. CO = cardiac output; HR = heart rate; SV= stroke volume
Vascular resistance, dictated by blood vessel diameter and elasticity, opposes blood flow. Constriction or elasticity loss raises resistance, elevating pressure, while dilation lowers resistance, reducing pressure.
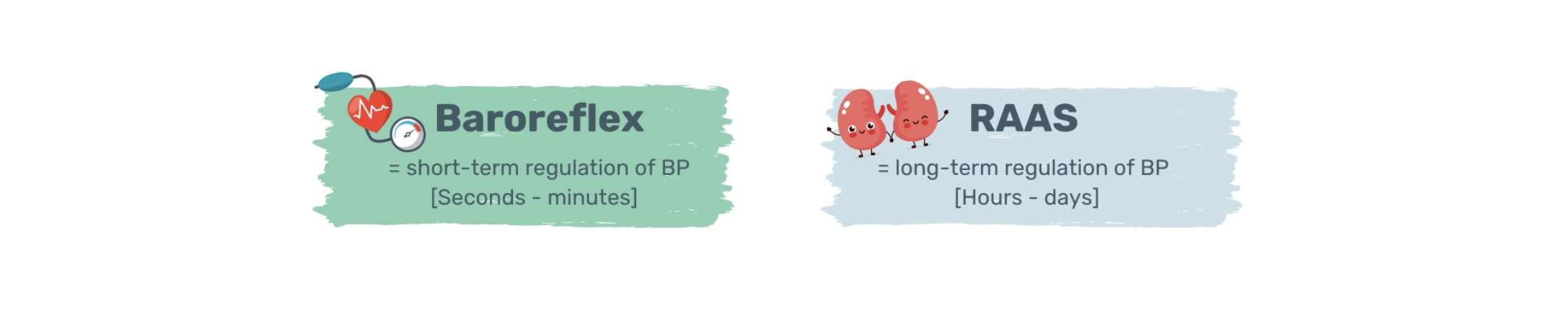
Tight regulation of cardiac output and vascular resistance maintains stable blood pressure. Pressure sensors within the arterial lumen, known as baroreceptors, continually monitor arterial pressure. This constant surveillance, known as baroreflex, allows rapid adjustments, normalising blood pressure within seconds to minutes.
Image: Cardiovascular centres. Located in the medulla oblongata, cardiovascular centres regulate cardiac output. They form part of the autonomic nervous system.
If arterial pressure rises, baroreceptor activity increases. This amplified signal travels to the vascular centres in the brain stem. In response, these centres reduce sympathetic and increase parasympathetic activity. Arteries and veins dilate, lowering vascular resistance and cardiac preload. Reduced preload leads to decreased diastolic heart filling, dropping cardiac output. Heightened parasympathetic activity further reduces heart rate and contractility, diminishing cardiac output.
Conversely, when arterial pressure drops, the baroreceptors’ activity decreases. This triggers the brain to activate the sympathetic and inhibit the parasympathetic nervous system. Arteries and veins constrict, increasing vascular resistance and cardiac preload. Consequently, cardiac output rises. Enhanced sympathetic activity accelerates heart rate and contractility, further augmenting cardiac output.
Image: Blood pressure control. The baroreflex is a short-term, fast response to changes in blood pressure. The renin-angiotensin-aldosterone system is a long-term, slow response. BP = blood pressure; RAAS = renin-angiotensin-aldosterone system
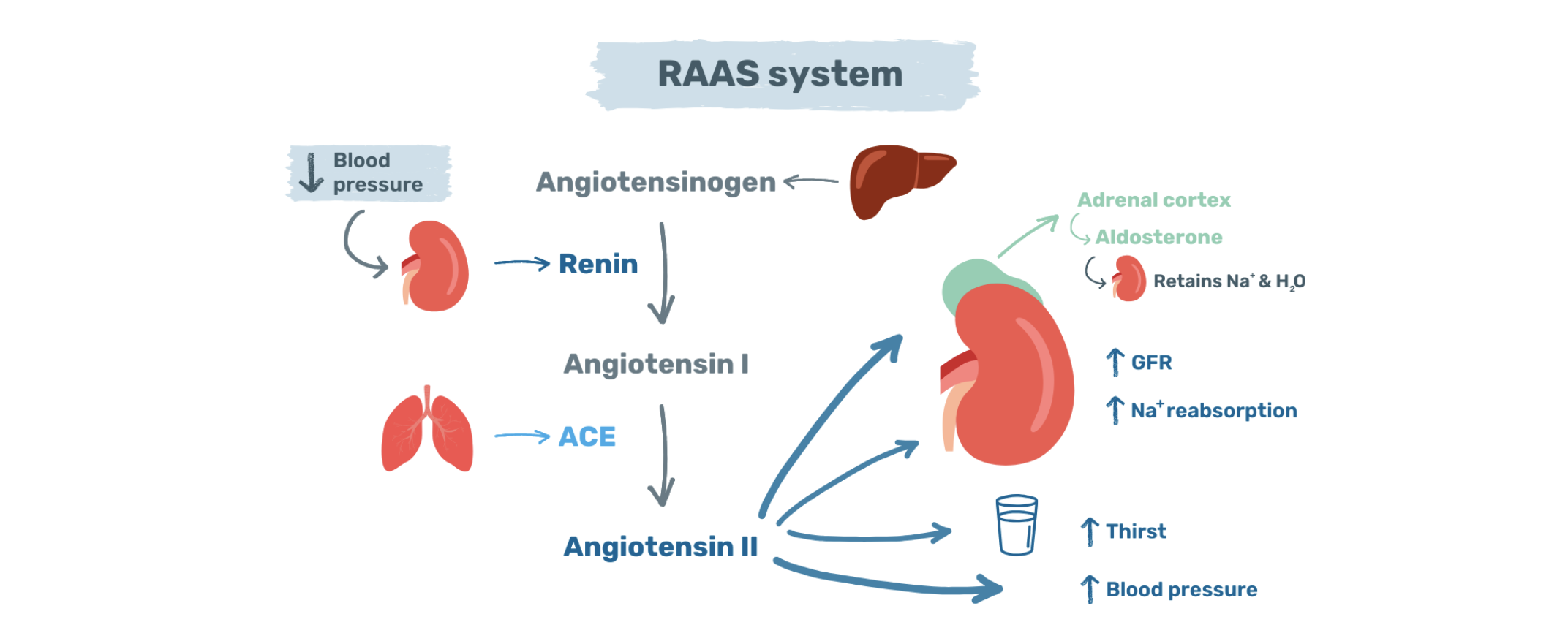
Another, albeit slower, blood pressure-lowering mechanism is the renin-angiotensin-aldosterone system. This system regulates blood volume by overseeing kidney fluid and sodium balance. When blood pressure or volume dips, the kidneys release the enzyme renin.
Renin activates angiotensin II, a potent blood pressure regulator, which promotes vasoconstriction, increases glomerular filtration rate and triggers sodium reabsorption. It also prompts aldosterone release, leading to sodium and water retention, and raising blood volume and pressure.
Image: Renin-angiotensin-aldosterone system. This network regulates blood pressure and volume for the long term. It consists of hormones, enzymes, and proteins. RAAS = renin-angiotensin-aldosterone system; GFR = glomerular filtration rate; Na+ = sodium; H2O = water
Pathophysiology of salt-induced hypertension
Hypertension classification varies across nations. European guidelines label blood pressure ≥ 140/90 mmHg as hypertensive, while American standards set it at ≥ 130/80 mmHg (4). Using the ≥140/90 mmHg threshold, nearly one in four adults fall into the high blood pressure category.
Hypertension is often called the silent killer as it develops without symptoms. It can take years or decades until organ damage becomes apparent. Routine blood pressure checks are crucial (5).
The risk of developing hypertension increases with age; by 80-85, 90% may be hypertensive (6). However, age is not the sole risk factor; unhealthy habits play a pivotal role. Excessive sodium intake, smoking, alcohol consumption, a sedentary lifestyle, obesity, and an unhealthy diet all contribute to elevated blood pressure (7).
Image: Risk factors. Non-modifiable and modifiable risk factors for hypertension at a glance. Please note that these lists are not exhaustive.
While sodium is essential, excessive consumption can trigger hypertension by causing water retention. Initially, the kidneys respond by excreting excess sodium and water. However, persistent high salt intake activates the local renin-angiotensin-aldosterone system within the kidneys (8). Aldosterone, responsible for sodium retention, also stimulates the production of reactive oxygen species. These, in turn, ignite oxidative stress, inflammation, fibrosis, and, ultimately, kidney failure (9).
Excess salt causes great damage beyond the kidneys, impairing the innermost lining of arteries, known as endothelium. Damaged endothelial cells produce less nitric oxide, leading to blood vessel constriction and promoting vascular inflammation (10). Inflamed arteries lose their elasticity, rendering them more susceptible to atherosclerosis (11).
Routine screenings are the only way to identify and address high blood pressure. If left untreated, hypertension can lead to serious complications including heart disease or stroke. However, early detection and lifestyle changes effectively reverse this silent threat.
Nutrition as a solution
A whole food plant-based diet effectively manages hypertension. Dark leafy greens like spinach, are rich in nitrates. Dietary nitrates enhance vasodilation and reduce arterial stiffness (12).
The Danish Diet Cancer and Health study tracked 53,000 people for 23 years. Those with the highest vegetable nitrate intake had lower blood pressure than those with the lowest intake. The decrease in blood pressure followed a linear dose-response pattern (13).
However, nitrates are not the only blood-pressure-lowering nutrients offered by plants. Plants are full of antioxidants such as vitamin E, vitamin C, beta-carotene, polyphenols, and omega-3 fatty acids. These compounds neutralise free radicals, mitigating oxidative stress and vascular inflammation (14).
The scientific consensus is clear: Plants help achieve healthy blood pressure and keep arteries strong and elastic. In a 2013 review of 32 studies, vegetarians showed lower systolic (6.9 mmHg) and diastolic (4.7 mmHg) blood pressures than omnivores (15).
While these reductions might appear modest, they hold significant health implications. Reducing systolic blood pressure by just 5 mmHg can cut stroke risk by 14%, heart disease by 9%, and overall mortality by 7% (16).
The Cardia hypertension study linked increased nut, fruit, whole grain consumption to lower blood pressure. In contrast, higher meat intake increased blood pressure (17). These findings are supported by the Epic-Oxford Study and Adventist Health Study-2 (AHS-2) (18,19). In both of these populations, vegans showed consistently lower blood pressure.
Another diet known for its blood-pressure-lowering effects is the Dietary Approach to Stop Hypertension (DASH) diet. Like the Mediterranean diet, the DASH diet is predominantly whole food, plant-based, low in saturated and trans fats. It promotes whole grains, vegetables, fruit, legumes, nuts and seeds and modest low-fat dairy, lean meat, and omega-3-rich fish. The DASH diet emphasizes reduced sodium and increased potassium intake. It also encourages the consumption of calcium-rich plant foods.
Potassium, vital for various physiological functions, helps relax arteries and counteracts the effects of sodium (20). Increased potassium intake leads to increased urinary sodium excretion (21). Moreover, it reduces heart disease risk and lowers blood pressure readings in hypertensive subjects (22,23).
Image: DASH diet. A predominantly plant-based diet to help prevent or treat hypertension. DASH = Dietary Approach to Stop Hypertension
Take-home message
Whole plant foods, low in sodium and saturated fat, are packed with blood pressure-lowering minerals like calcium, magnesium, and potassium. But that’s not all. Plants assist in weight loss by reducing calorie intake. For every kilogram lost, blood pressure can decrease by 1 mmHg (24).
Ready to guide your patient towards healthier eating? Explore our tips below.
Tips for encouraging healthy eating in your patients
Go plant-based: Try whole food plant-based diets like the DASH.
Stock up on nitrates: Add leafy greens and beetroot for a healthier approach.
Watch the salt: Cut back on processed, salty foods and eat out less.
Monitor progress: A healthy diet often means better blood pressure.
Trim down: Plants can help maintain or reach a healthy body weight.
Beyond a healthy diet, 150 minutes of moderate exercise a week can also help your patient fight hypertension.
Additional Information:
-
Dr Miriam Sonntag is the Medical Content Executive of the online learning platform, PAN Academy. Having worked in basic research, she knows how to decipher complex information. Working now at PAN, she scans and pours over scientific papers and books. She breaks down the latest nutritional research into actionable advice for everyday life. She is committed to sharing the bigger picture of why it is good to put more plants on your plate.
-
For more information on this topic, download the Hypertension and Diet factsheet for physicians.
-
WHO. Hypertension. Last accessed: 8 January 2024. Available from: https://www.who.int/health-topics/hypertensionCuspidi et al., 2018. Treatment of hypertension: The ESH/ESC guidelines recommendations.Available from: https://www.sciencedirect.com/science/article/pii/S1043661817311179
American Heart Association. Understanding Blood Pressure Readings. Last accessed: 14 December 2023. Available from: https://www.heart.org/en/health-topics/high-blood-pressure/understanding-blood-pressure-readings
Whelton et al.,2022. Harmonization of the American College of Cardiology/American Heart Association and European Society of Cardiology/European Society of Hypertension Blood Pressure/Hypertension Guidelines: Comparisons, Reflections, and Recommendations. Available from: https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.121.054602
WHO. Hypertension. Last accessed: 8 January 2024. Available from: https://www.who.int/news-room/fact-sheets/detail/hypertension
National High Blood Pressure Education Program, 2004. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Available from: http://www.ncbi.nlm.nih.gov/books/nbk9630/
Carey et al., 2018. Prevention and control of hypertension: JACC health promotion series. Available from: https://doi.org/10.1016/j.jacc.2018.07.008
Klabundle, 2022. CV Physiology | Renin-Angiotensin-Aldosterone System. Available from: https://cvphysiology.com/blood-pressure/bp015
Brown, 2013. Contribution of aldosterone to cardiovascular and renal inflammation and fibrosis. Available from: https://doi.org/10.1038/nrneph.2013.110
Alexander et al., 2021. Endothelial function in cardiovascular medicine: a consensus paper of the European Society of Cardiology Working Groups on Atherosclerosis and Vascular Biology, Aorta and Peripheral Vascular Diseases, Coronary Pathophysiology and Microcirculation, and Thrombosis. Available from: https://doi.org/10.1093/cvr/cvaa085
Touyz et al.,2018. Vascular smooth muscle contraction in hypertension. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5852517/
Jovanovski et al., 2015. Effect of Spinach, a High Dietary Nitrate Source, on Arterial Stiffness and Related Hemodynamic Measures: A Randomized, Controlled Trial in Healthy Adults. Available from: https://doi.org/10.7762%2Fcnr.2015.4.3.160
Bondonno et al., 2021. Vegetable nitrate intake, blood pressure and incident cardiovascular disease: Danish Diet, Cancer, and Health Study. Available from: https://doi.org/10.1007/s10654-021-00747-3
Kim et al., 2012. Long-term vegetarians have low oxidative stress, body fat, and cholesterol levels. Available from: https://doi.org/10.4162%2Fnrp.2012.6.2.155
Yokoyama et al., 2014. Vegetarian Diets and Blood Pressure: A Meta-analysis. Available from: https://doi.org/10.1001/jamainternmed.2013.14547
Verma et al., 2021. Non‐pharmacological management of hypertension. J Clin Hypertens. Available from: https://doi.org/10.1111%2Fjch.14236
Steffen et al., 2005. Associations of plant food, dairy product, and meat intakes with 15-y incidence of elevated blood pressure in young black and white adults: the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Available from: https://doi.org/10.1093/ajcn/82.6.1169
Appleby et al., 2002. Hypertension and blood pressure among meat eaters, fish eaters, vegetarians and vegans in EPIC–Oxford. Available from: https://doi.org/10.1079/phn2002332
Pettersen et al., 2012. Vegetarian diets and blood pressure among white subjects: results from the Adventist Health Study-2 (AHS-2). Available from: https://doi.org/10.1017/s1368980011003454
Yamada & Inaba, 2021. Potassium metabolism and management in patients with CKD. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8224083/
Lin et al., 2012. Blood pressure-lowering mechanisms of the DASH dietary pattern. Available from: https://doi.org/10.1155/2012/472396
O’Donnell et al., 2014. Urinary sodium and potassium excretion, mortality, and cardiovascular events. Available from: https://doi.org/10.1056/nejmoa1311889
Poorolajal et al., 2017. Oral potassium supplementation for management of essential hypertension: a meta-analysis of randomized controlled trials. Available from: https://doi.org/10.1371/journal.pone.0174967
Neter et al., 2003. Influence of Weight Reduction on Blood Pressure. Available from: https://www.ahajournals.org/doi/10.1161/01.hyp.0000094221.86888.ae