Heart Disease Uncovered: A Physician’s Guide
By Dr. Miriam Sonntag from the PAN Academy – our online learning platform where you can learn all about nutrition and health.
Heart disease – the umbrella term
Heart disease, the leading cause of illness and death, claims 56.5 million lives worldwide per year. In the US alone, a person dies every 33 seconds (1). Across Europe, it contributes to 45% of all deaths (2) – a staggering 3.9 million lives each year.
Image: Heart disease. A group of heart and blood vessel disorders. Some are present at birth, while others develop over a lifetime. Many are linked to atherosclerosis.
Heart disease, also known as cardiovascular disease, is an umbrella term. It describes various disorders affecting the heart and vascular system. This blog post focuses on the most prevalent form: coronary artery disease.
We’ll dive into the roots of an atherosclerotic heart attack and discover that many cases are not just preventable but also reversible. Gain insight into how adopting a whole food, plant-based diet can help your patients towards a heart-healthy life.
Atherosclerosis – the underlying disease
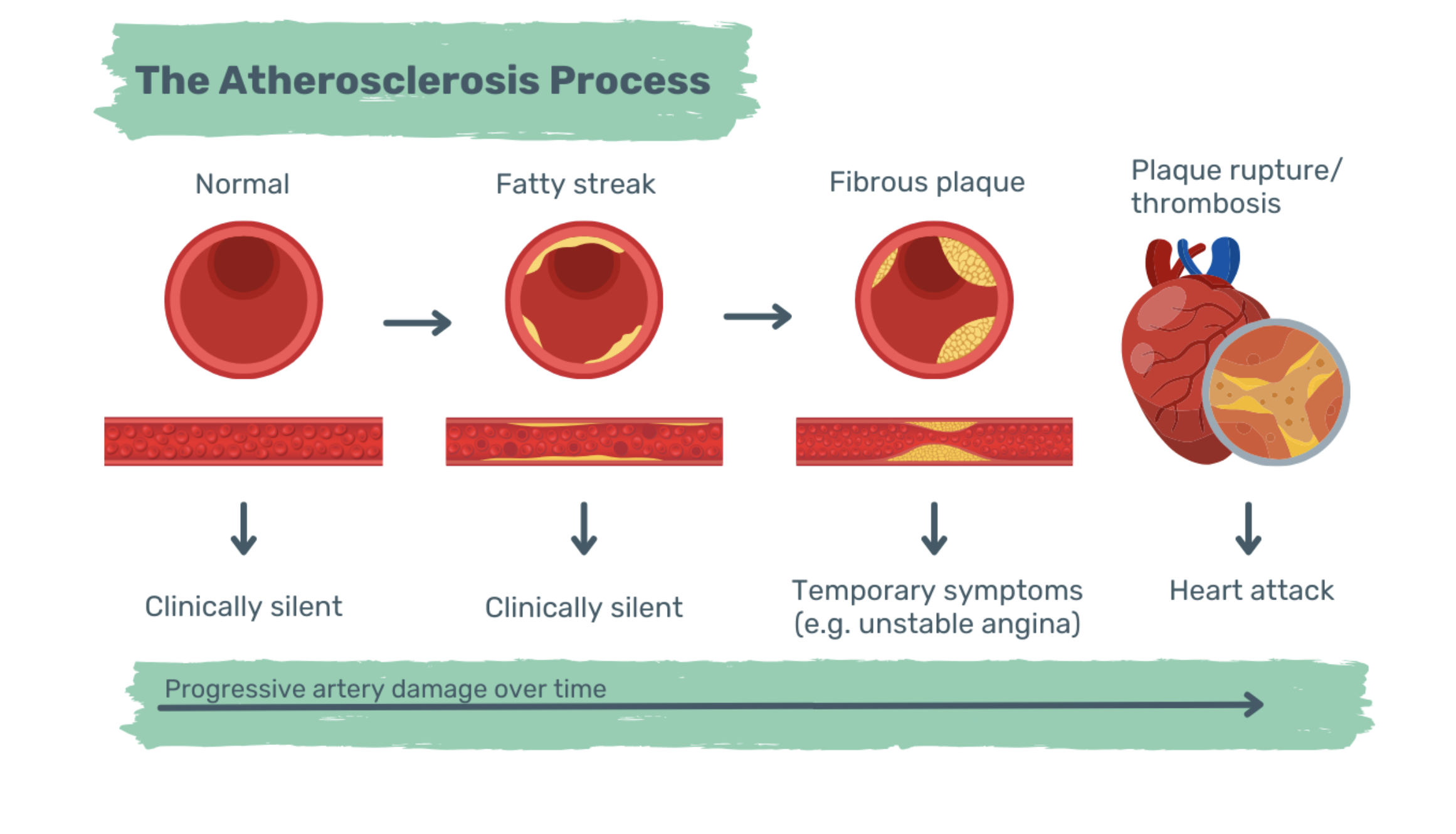
A heart attack, or myocardial infarction, isn’t a disease. It’s the final stage of atherosclerosis – a stepwise process of blood vessel hardening, narrowing, and inflammation. Years of accumulating harm eventually result in a fully blocked coronary artery. With no oxygen-rich blood flowing through the blocked artery, the heart muscle becomes ischemic and starts to die.
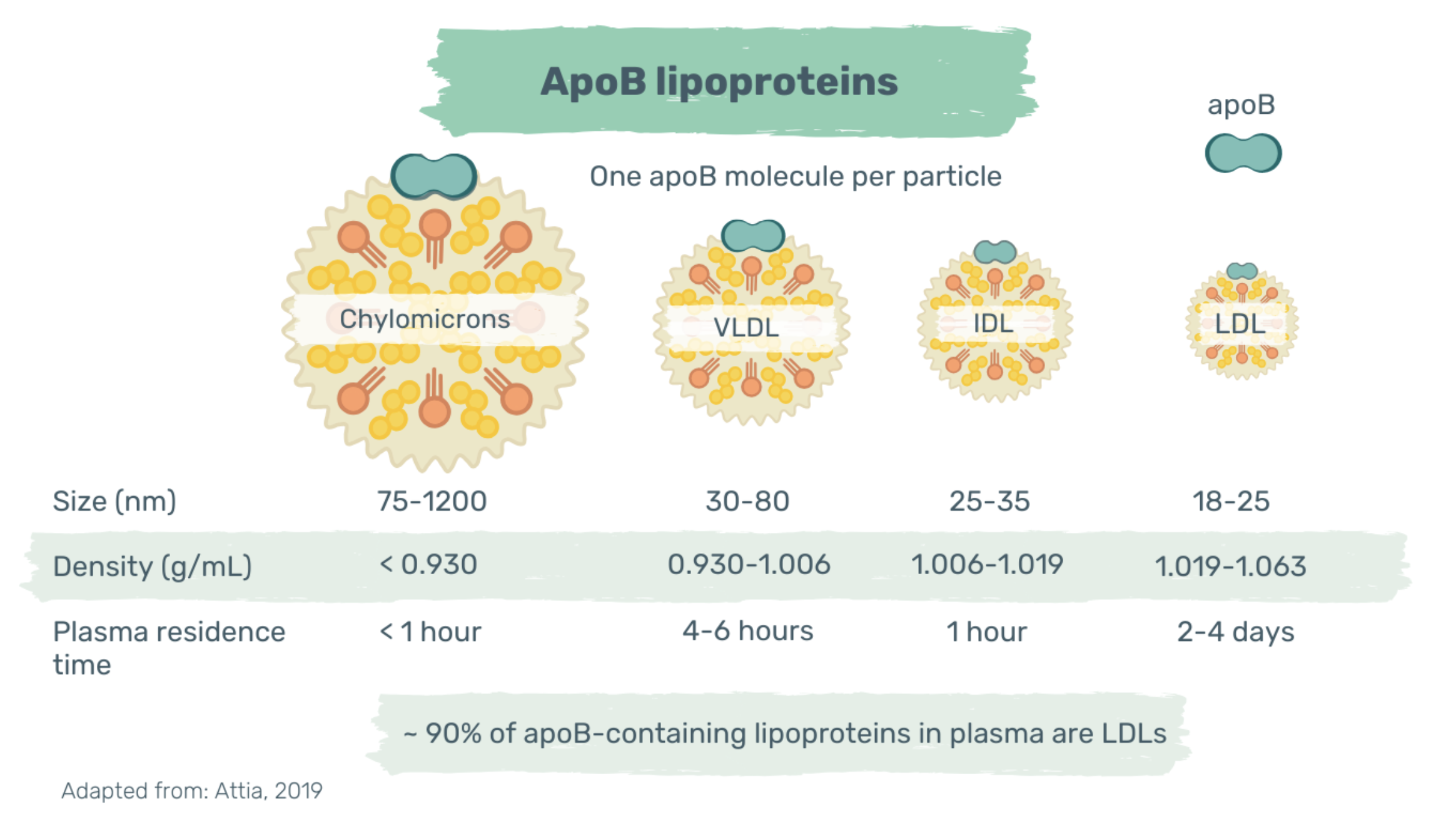
The narrowing and hardening of arteries start decades before the acute event. Apolipoprotein B (apoB)-containing lipoproteins infiltrate the artery wall and accumulate over time. At physiological levels (20-40mg/dl), apoB particles, with a diameter < 70nm, can freely enter and exit the artery wall (3). However, when plasma levels exceed this threshold, dose-dependent retention of cholesterol-rich, apoB-containing lipoproteins occurs in the artery wall.
Image: ApoB-containing lipoproteins. Cholesterol-rich apoB-containing lipoproteins include chylomicrons, VLDL, IDL and LDL. Each of these particles contains one single apoB-molecule. ApoB = apolipoprotein B; VLDL = very low-density lipoprotein, IDL = intermediate-density lipoprotein, LDL = low-density lipoprotein. Read more: Attia, 2019 and Sniderman et al., 2019]
Once trapped, apoB-containing lipoproteins are modified by artery-wall enzymes and oxidation. Modified lipoproteins tend to aggregate and trigger a maladaptive immune response (4). Immune cells, mainly monocytes, are recruited and endothelial cells increase the production of reactive oxygen species. High levels of reactive oxygen species further increase lipid oxidation.
Image: Initiation and fatty streak formation. High plasma concentrations of apoB-containing lipoproteins (< 70nm in diameter) drive the fatty streak formation. The retained cholesterol-containing particles become modified and tend to aggregate. Monocytes infiltrate the artery wall, transform into macrophages, and internalise aggregated LDL particles. Macrophages turn into cholesterol-laden foam cells. ROS = reactive oxygen species; LDL = low-density lipoprotein. Image taken from: Linton et al., 2019]
The recruited and retained monocytes differentiate into macrophages. By absorbing aggregated lipoproteins, macrophages turn into cholesterol-laden foam cells. The build-up of foam cells creates a fatty streak between the tunica intima and the tunica media of the artery.
Image: Artery wall structure. The artery wall has three distinct layers.
Fatty streaks are clinically silent and can regress with lifestyle changes. Yet, prolonged exposure to high levels of apoB-containing lipoproteins can transform them into fibrous plaque, also known as atheromas. Vascular smooth muscle cells migrate to the tunica intima and create a fibrous coating. This thick cap acts as a protective barrier against plaque rupture (5).
Moreover, excessive cholesterol loading sparks macrophage inflammation; oxidative stress and foam cell number increases. Unresolved inflammation leads to vulnerable plaques with increased macrophage cell death (6). A necrotic core forms as apoptotic cells are not efficiently cleared. Dying macrophages release lipids and provoke more inflammation, oxidation and smooth muscle cell death (5).
As the necrotic core grows, the fibrous cap weakens and eventually ruptures (7). When a plaque breaks open, a clot forms. This thrombus may clot and close the entire artery, resulting in a myocardial infarction or even death. In earlier stages, when the artery is significantly narrowed, symptoms such as chest pain, shortness of breath and fatigue may become apparent. To maintain or regain vascular health, early detection and intervention are key.
Image: The atherosclerosis process. It’s a stepwise process. In the early, subclinical stage the blood vessel lumen remains open. However, as the disease advances, the blood vessel lumen gradually narrows until it closes completely. A narrowed or closed artery fails to deliver an adequate amount of oxygen to the heart muscle. Early signs of an ischemic heart muscle are chest pain, shortness of breath and fatigue.
The two biggest risk factors
The science is pretty clear: the higher the apoB plasma concentration, the greater the risk of atherosclerotic heart disease. It’s a dose-dependent, log-linear association.
In most people, 90% of circulating apoB-containing lipoproteins are LDL particles (3). In clinical practice, plasma LDL levels are estimated by measuring LDL-cholesterol, the total amount of cholesterol in LDL particles. Plasma LDL-cholesterol levels usually correlate with LDL particle numbers. However, under certain conditions like hypertriglyceridemia or metabolic syndrome, these values may become discordant. Thus, to accurately assess the risks of atherosclerotic plaque formation, it’s best to measure both plasma LDL-cholesterol and apoB concentration (8).
Current guidelines recommend LDL-cholesterol levels below 100 mg/dL (2.6 mmol/L) in healthy patients, a target validated by a 30% risk reduction in cardiovascular mortality (9). LDL-cholesterol levels at 130 mg/dL (3.4 mmol/L) or higher increases the risk by 50% (10).
However, a growing body of evidence suggests maintaining even lower LDL-cholesterol levels, ideally within the range of 50-70 mg/dl (1.3 – 1.8 mmol/L) (11). This physiologically normal range prevents fat and cholesterol accumulation in the artery wall.
For individuals with established atherosclerotic cardiovascular disease, achieving LDL-cholesterol levels below 70 mg/dl (1.8 mmol/L) has been shown to arrest and reverse atheromas (12). These findings resonate with the targeted LDL-cholesterol values recommended by the European Society of Cardiology. They advocate for levels < 70 mg/dl (1.8 mmol/L) in high-risk and < 55 mg/dL (1.4 mmol/L) in very high-risk-patients (9).
Besides high circulating apoB levels, hypertension plays another key role. It accounts for around 50% of all cardiovascular disease deaths (13). Elevated blood pressure forces the heart to work harder. Both, the oxygen demand and risk of heart muscle ischemia increase. Increased arterial pressure leads to increased vascular contraction and arterial remodelling. The inner lining, called endothelium, gets damaged and is more likely to develop atherosclerosis (14).
With high LDL-cholesterol and blood pressure as the top risk factors, heart disease is primarily a lifestyle-related condition. We can eradicate atherosclerotic heart disease via early detection and intervention. The American Heart Association estimates that around 80% of cardiovascular diseases can be prevented (15).
Nutrition as a solution
Adopting a whole food plant-based diet can help achieve targeted LDL-cholesterol levels below 70 mg/dl (1.8 mmol/L). Compelling evidence suggests that fewer animal products lead to better outcomes. Vegans tend to be leaner, have lower cholesterol levels, better glucose control, and reduced blood pressure compared to omnivores (16).
In 1993, the Lyon Heart Study showed that following a Mediterranean diet lowers the risk of heart attacks by 72% (17). Likewise, during a 2018 study spanning two years, heart-disease-free participants saw a 30% lower risk of heart attack by following the Mediterranean diet (18).
Eating more unprocessed plants not only keeps arteries healthy, strong, and elastic; but can also reverse atherosclerosis. The Lifestyle Heart Trial demonstrated that a predominantly plant-based diet, along with exercise and stress management, can heal damaged arteries. Patients in the intervention group lowered angina frequency by 91%, reduced stenosis by 5% and dropped LDL-cholesterol values by 34.7% (19).
In 2014, these remarkable results were backed up. In a case study of 198 heart patients, an oil-free plant-based diet was key. Of 177 who followed the diet for 4 years, only one had a non-fatal stroke. Whereas 62% of those who didn’t follow the diet, experienced adverse events like heart attacks or stroke. Whole food, plant-based eaters showed reversed atherosclerotic plaques and renewed artery lining (20).
Image: Coronary angiography. Angiogram before and after 32 months on a plant-based diet, without cholesterol-lowering medication. The previously diseased distal left anterior descending artery has returned to its normal configuration.
Unprocessed plants are cholesterol-free, low in saturated fats, refined carbohydrates, and sodium. Animal products and processed foods are usually the opposite. Replacing just 5% of dairy fat calories with whole grains can lower your cardiovascular disease risk by 28% (21). Yet, swapping saturated fats from dairy or meat with white bread and other refined carbohydrates may increase your risk (22).
Moreover, plant foods are packed with antioxidants and fibre. Adding just 10 grams of fibre per day can cut the risk of heart disease by 17% (23). Fibre from whole foods forms the foundation of a healthy gut. It keeps healthy microbes well-fed and helps to lower LDL-cholesterol and decrease blood pressure (24).
On the flip side, animal products can damage or disrupt the microbiome. They feed inflammatory microbes, which produce the toxic metabolite trimethylamine N-oxide (TMAO). Increased TMAO means increased vascular inflammation. Prolonged elevated circulating levels of TMAO impair vascular endothelial function (25). Consequently, the artery becomes more susceptible to atherosclerosis.
Antioxidants vitamin E, vitamin C, beta-carotene, and polyphenols mainly act as radical scavengers (26). They reduce reactive oxygen species and thus protect LDL-cholesterol particles from being oxidised and trapped in macrophages (5). Moreover, plant foods abundant in nitrates and polyphenols enhance nitric oxide production (27,28).
Nitric oxide has strong vasodilatory, anti-inflammatory, and antioxidant properties. It plays a central role in vascular homeostasis (28). A healthy vascular endothelium is less atherosclerosis-prone.
Take-home message
Whole plant foods not only prevent arteries from clogging but may arrest and reverse existing atherosclerosis. By being naturally low in sodium and cholesterol-free, plant foods combat the two biggest cardiovascular disease risk factors – high blood pressure and high circulating LDL-cholesterol.
Tips for encouraging healthy eating in your patients
Pick healthy fats: Swap saturated fats with healthy, unsaturated fats.
Eat the rainbow: Aim for 30 or more different plant foods per week.
Increase fibre intake: Swap refined grains with whole grains and add legumes.
Enjoy antioxidant-rich foods: Include garlic, olive oil, soy products, and turmeric.
Add nitrate-rich foods: Include green leafy vegetables and red beetroot.
Limit ultra-processed foods: Limit junk food and refined carbs.
Ready to unveil the benefits of a whole food, plant-based diet to your patients? Explore our tips above together with them and start with the easiest and most impactful change for them.
Additional Information:
-
Dr Miriam Sonntag is the Medical Content Executive of the online learning platform, PAN Academy. Having worked in basic research, she knows how to decipher complex information. Working now at PAN, she scans and pours over scientific papers and books. She breaks down the latest nutritional research into actionable advice for everyday life. She is committed to sharing the bigger picture of why it is good to put more plants on your plate.
-
For more information on this topic, download the Heart Disease and Diet factsheet for patients.
For more information on this topic, download the Heart Disease and Diet factsheet for physicians.
-
Centers for Disease Control and Prevention, 2022. LDL and HDL cholesterol and triglycerides. Available from: https://www.cdc.gov/cholesterol/ldl_hdl.htm (Accessed 6 Mar 2023).
European Heart Network. European cardiovascular disease statistics 2017. Available from: https://ehnheart.org/about-cvd/the-burden-of-cvd/ (Accessed 17 Jun 2023)
Ference et al., 2017. Low-density lipoproteins cause atherosclerotic cardiovascular disease. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. Available from: https://doi.org/10.1093/eurheartj/ehx144
Ruuth et al., 2018. Susceptibility of low-density lipoprotein particles to aggregate depends on particle lipidome, is modifiable, and associates with future cardiovascular deaths. Available from: https://academic.oup.com/eurheartj/article/39/27/2562/5049093?login=false#377899879
Linton et al., 2019. The role of lipids and lipoproteins in atherosclerosis. Available from: https://www.ncbi.nlm.nih.gov/sites/books/NBK343489/
Moore et al., 2013. Macrophages in atherosclerosis: a dynamic balance. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4357520/
Gui et al., 2022. Foam cells in atherosclerosis: novel insights into its origins, consequences, and molecular mechanisms. Available from: https://www.frontiersin.org/articles/10.3389/fcvm.2022.845942/full
Sniderman et al., 2011. A meta-analysis of low-density lipoprotein cholesterol, non-high-density lipoprotein cholesterol, and apolipoprotein B as markers of cardiovascular risk. Available from: https://www.ahajournals.org/doi/10.1161/CIRCOUTCOMES.110.959247
Visseren et al., 2021. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice: developed by the task force for cardiovascular disease prevention in clinical practice with representatives of the European Society of Cardiology and 12 medical societies with the special contribution of the European Association of Preventive Cardiology (EAPC). Available from: https://doi.org/10.1093/eurheartj/ehab484
Abdullah et al., 2018. Long-term association of low-density lipoprotein cholesterol with cardiovascular mortality in individuals at low 10-year risk of atherosclerotic cardiovascular disease. Available from: https://www.ahajournals.org/doi/full/10.1161/CIRCULATIONAHA.118.034273
O’Keefe et al., 2004. Optimal low-density lipoprotein is 50 to 70 mg/dl: lower is better and physiologically normal. Available from: https://www.jacc.org/doi/full/10.1016/j.jacc.2004.03.046
Nicholls et al., 2016. Effect of evolocumab on progression of coronary disease in statin-treated patients: the GLAGOV randomized clinical trial. Available from: https://jamanetwork.com/journals/jama/fullarticle/2584184
WHO. World health report : 2002 [Internet]. [cited 2023 Aug 25]. Available from: https://www.who.int/publications-detail-redirect/9241562072
Touyz et al., 2018. Vascular smooth muscle contraction in hypertension. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5852517/
Benjamin et al., 2019. Heart disease and stroke statistics-2019 Update: a report from the American Heart Association. Available from: https://doi.org/10.1161/CIR.0000000000000659
Benatar & Stewart, 2018. Cardiometabolic risk factors in vegans; a meta-analysis of observational studies. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6301673/
de Lorgeril et al., 1999. Mediterranean diet, traditional risk factors, and the rate of cardiovascular complications after myocardial infarction. Available from: https://www.ahajournals.org/doi/10.1161/01.cir.99.6.779
Estruch et al., 2018. Primary prevention of cardiovascular disease with a Mediterranean diet supplemented with extra-virgin olive oil or nuts. Available from: https://pubmed.ncbi.nlm.nih.gov/29897866/
Ornish et al., 1990. Can lifestyle changes reverse coronary heart disease? The Lifestyle Heart Trial. Available from: https://pubmed.ncbi.nlm.nih.gov/1973470/
Esselstyn et al., 2014. A way to reverse CAD? Available from: https://www.mdedge.com/familymedicine/article/83345/cardiology/way-reverse-cad
Chen et al., 2016. Dairy fat and risk of cardiovascular disease in 3 cohorts of US adults. Available from: https://doi.org/10.3945/ajcn.116.134460
Liu et al., 2017. A healthy approach to dietary fats: understanding the science and taking action to reduce consumer confusion. Available from: https://doi.org/10.1186/s12937-017-0271-4
Liu et al., 2015. Fiber consumption and all-cause, cardiovascular, and cancer mortalities: a systematic review and meta-analysis of cohort studies. Available from: https://onlinelibrary.wiley.com/doi/10.1002/mnfr.201400449
Hartley et al., 2016. Dietary fibre for the primary prevention of cardiovascular disease. Available from: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD011472.pub2/full
Zhu et al., 2020. Gut microbiota in atherosclerosis: focus on trimethylamine N-oxide. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1111/apm.13038
Kim et al., 2012. Long-term vegetarians have low oxidative stress, body fat, and cholesterol levels. Available from: https://pubmed.ncbi.nlm.nih.gov/22586505/
Serreli & Deiana, 2023. Role of dietary polyphenols in the activity and expression of nitric oxide synthases: a review. Available from: https://www.mdpi.com/2076-3921/12/1/147
Cyr et al., 2020. Nitric oxide and endothelial dysfunction. Available from: https://pubmed.ncbi.nlm.nih.gov/32172815/
Attia , 2019. Measuring cardiovascular disease risk and the importance of apoB. Available from: https://peterattiamd.com/measuring-cardiovascular-disease-risk-and-the-importance-of-apob-part-1/ [Accessed 18 Jan 2024]
Sniderman et al., 2019. Apolipoprotein b particles and cardiovascular disease: a narrative review. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7369156/