Beyond the Scale: Understanding Obesity for Medical Students
By Dr. Miriam Sonntag from the PAN Academy – our online learning platform where you can learn all about nutrition and health.
The World Obesity Atlas unveils shocking numbers: In 2020, 38% of the world’s population, a staggering 2.6 billion people aged over five years, were overweight or obese. Even more alarming are the projections for 2035. 20% of children aged 5-19 years are expected to be obese (1). In this blog post, we will unlock the secrets of obesity. We’ll delve into the energy balance equation and unveil a simple strategy to combat this global epidemic.
Overweight and obesity
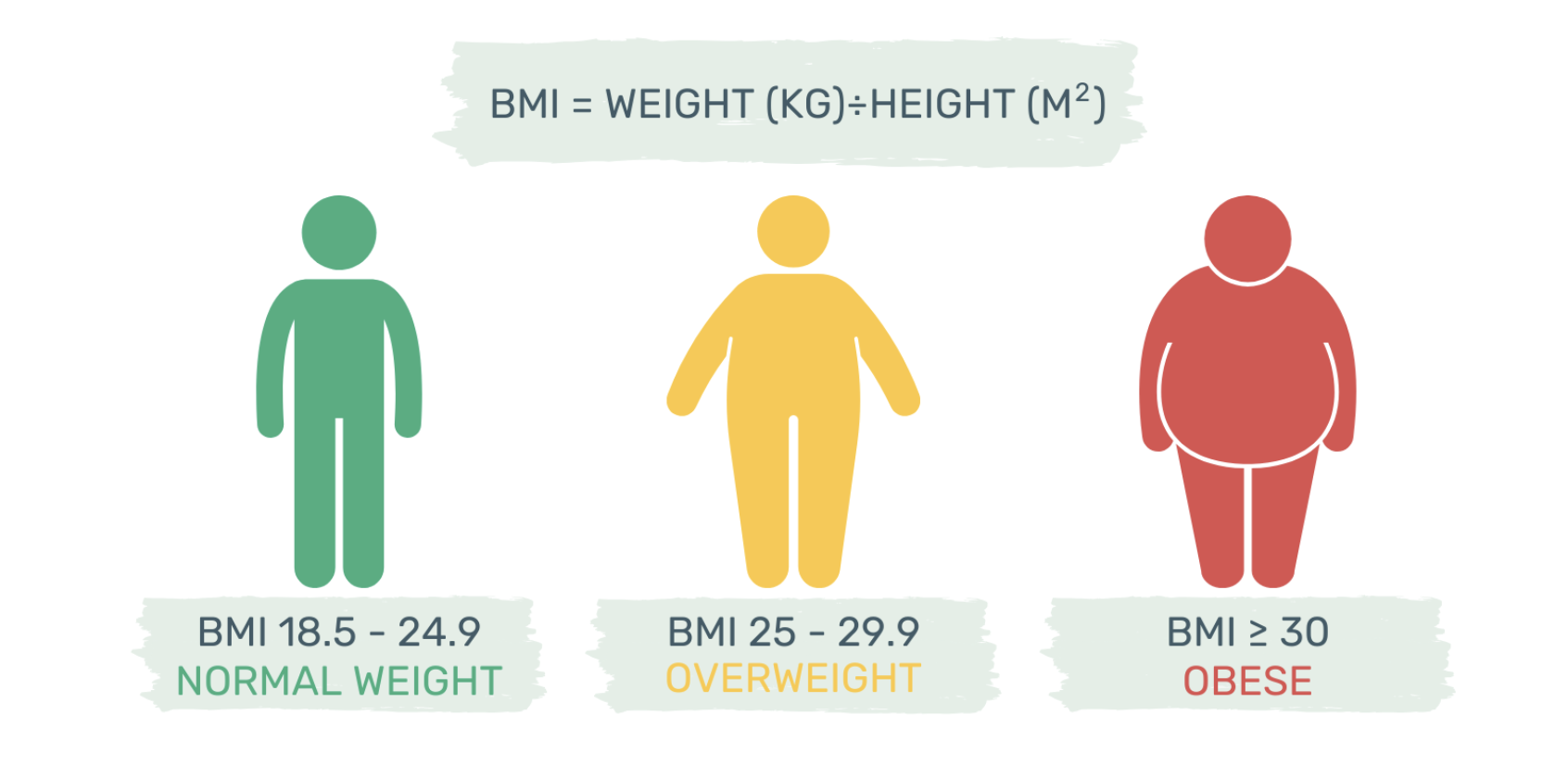
Overweight and obesity are defined as abnormal or excessive body fat. The World Health Organization uses the body mass index – BMI for short – to determine body fat percentage.
The BMI is the most useful indicator of overweight and obesity at the population level, yet it’s not perfect. It can’t differentiate between fat and muscle mass, nor does it state anything about the body fat distribution (2).
A growing body of evidence links excess abdominal and ectopic fat to an increased risk of chronic diseases (3,4). The equation is clear: the more intra-abdominal or visceral fat, the higher the risk. Abdominal fat correlates with waist circumference. To accurately assess health risks, it is best to combine BMI with the waist-to-height ratio (WHtR) (2).
Depending on their waist-to-height ratio, obese patients fall into two categories. Metabolically healthy (MHO) or unhealthy (MUO) obesity. A BMI ≥ 30 paired with a waist-to-height ratio below 0.5 indicates healthy central obesity or MHO. These patients have lower visceral and ectopic fat but higher subcutaneous limb fat. They show greater cardiovascular fitness and physical activity. Their adipose tissue functions properly, releasing less inflammatory cytokines compared to patients with metabolically unhealthy obesity (5).
Studies suggest that metabolically healthy obesity is a transient phenotype. Patients with MHO have a decreased risk of developing cardiometabolic diseases (CMD). But only in contrast to metabolically unhealthy obese patients, not to healthy lean individuals (6).
Pathomechanism of obesity
Obesity results from a positive energy balance. If you eat more calories than you burn, you gain fat. It doesn’t matter if the energy surplus comes from fat, carbohydrates, or protein. All calories are the same.
To store excess calories, the adipose tissue must expand. There are two ways fat depots respond to higher storage demands: By increasing the adipocyte number through adipogenesis from precursor cells, known as hyperplasia. Or through increasing the size of existing fat cells, known as hypertrophy (7).
As adipocytes expand, their oxygen supply decreases. Hypoxic stress induces adipocyte necrosis, and macrophage infiltration. Macrophages release interleukin 6 and TNF-alpha, two pro-inflammatory cytokines, creating low-grade chronic inflammation of adipose tissue. Indeed, studies suggest that the bigger fat cells become, the more pro-inflammatory cytokines they secrete.
Unresolved adipose tissue inflammation can also lead to fibrotic remodelling. Collagen accumulation around adipocytes hampers fat storage, leading to elevated blood triglyceride levels (8). These circulating free fatty acids can then infiltrate the liver, muscle, and pancreas, forming ectopic fat stores.
It’s a vicious circle. Excess body fat creates inflammation, and inflammation promotes toxic fat accumulation in non-adipose tissues. Excess lipids in non-adipose tissue lead to various comorbidities like type 2 diabetes, cardiovascular disease, and certain cancers (9).
Fat loss physiology
The energy balance equation states that long-term changes in adiposity depend on the calories consumed minus the calories expended (10). Therefore, to lose fat, we must cut calories, burn more, or do both. Although this concept seems straightforward, its application can be challenging. Let’s have a closer look.
The key to understanding the challenge of fat loss, lies in our hypothalamus. The hypothalamus detects and responds to fluctuating leptin and ghrelin levels – two opposing hormones. When leptin levels are high, the hypothalamus cranks up your metabolism and decreases your appetite (11). Leptin is secreted by fat cells. The more body fat you have, the more leptin you secrete.
In contrast, when we are in a negative energy balance, leptin levels decrease and ghrelin levels increase. Ghrelin is secreted by an empty stomach. The hypothalamus senses the altered leptin and ghrelin levels and activates the hunger circuitry. Our metabolism slows down, which lowers energy expenditure. And our hunger increases, driving us to find food.
Lower leptin levels push the hypothalamus to activate the hunger response. Yet, the precise threshold at which leptin will trigger the hunger circuitry is highly individual. It’s connected to your genes, eating habits and the typical leptin levels circulating in your blood (11).
There’s a growing body of evidence that the obesogenic environment we’re living in confuses our brain hormones (12). The hypothalamus cannot precisely match energy intake to expenditure. With all the flavoursome, highly processed foods, we tend to overeat calories. Not by much, but it adds up over time as fat.
Nutrition as a solution
There is strong evidence that maximising the amounts of whole plants in your diet can break the vicious circle. An ad libitum whole food plant-based diet reduces BMI by 4.4 compared to 0.4 on normal obesity care diet (13). Moreover, plant-based diets can lower obesity-related inflammation markers (14).
Unprocessed plants have a very low to low-calorie density. Plus, they are rich in fibre, which fuels your gut bacteria. Keeping your microbes well-fed means they produce a multitude of beneficial metabolites. Short-chain fatty acids, like butyrate, stimulate the production of leptin. Conversely, fibre-rich meals reduce ghrelin, an appetite-stimulating hormone.
As a result, you feel full while consuming fewer calories. Indeed, studies state that a low-calorie-density diet can offer satiety with half the calories of a high-calorie-density diet (15). In addition, calorie-dense ultra-processed meals facilitate overeating and the development of obesity. Consumed faster, these meals lead to a delayed sense of fullness and thus a higher total energy intake (16).
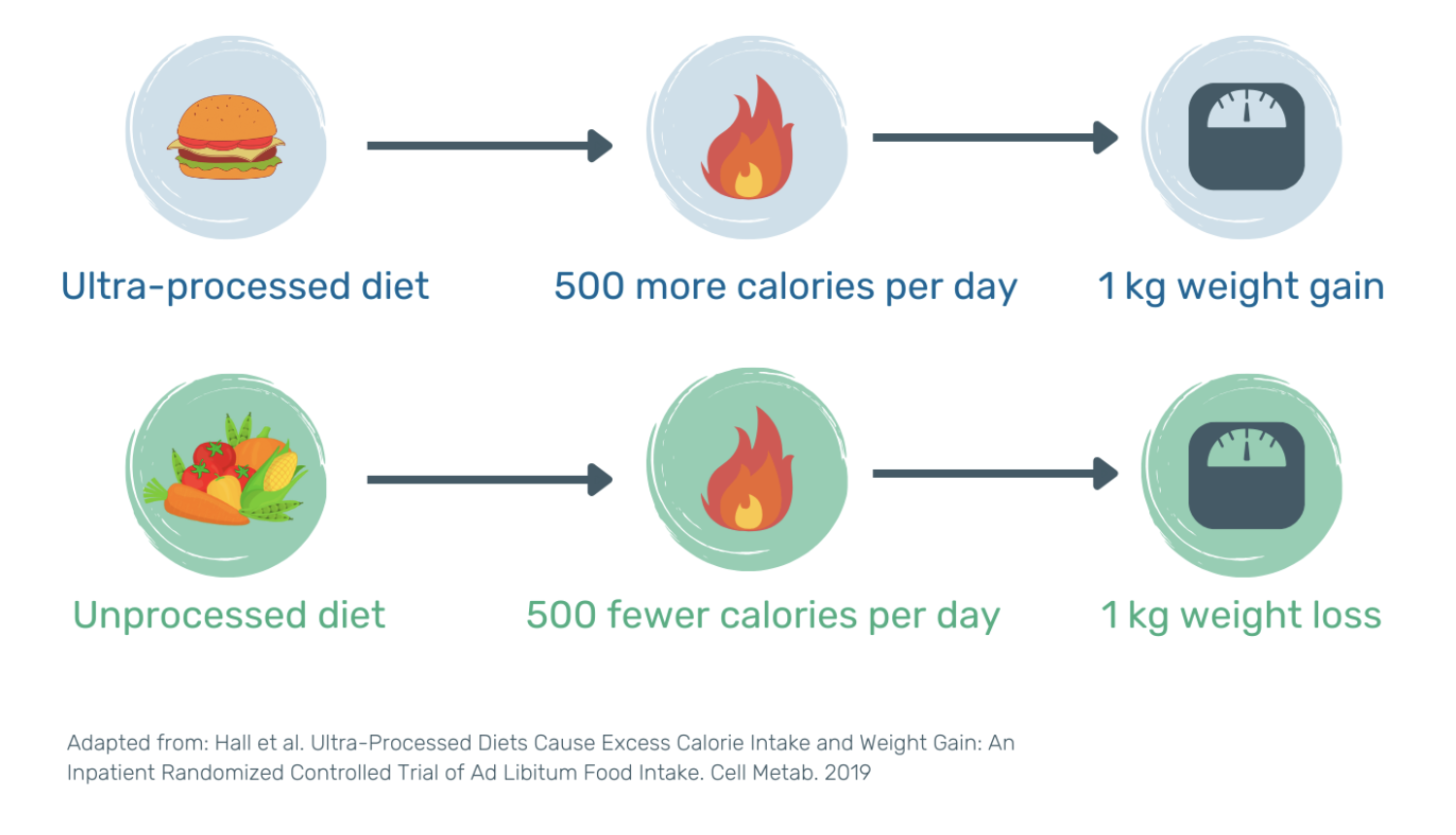
A 2019 cross-over study explored the effects of ultra-processed foods on energy intake and weight gain (12). Twenty overweight participants followed both an ultra-processed and unprocessed diet for 14 days each. Both diets were macronutrient, sugar, salt, and fibre matched. On the ultra-processed diet, participants overate 500 calories per day, causing a 1 kg weight gain. On the unprocessed diet, participants ate 500 fewer calories per day, resulting in a 1 kg weight loss.
Take-home message
Whole plant foods have a lower calorie density than ultra-processed and animal foods. They provide greater satisfaction while consuming fewer calories. Unprocessed plants create a calorie deficit or equilibrium. By maximising intake of whole plant foods, no calorie counting is required to achieve or maintain a healthy body weight.
Ready to unveil the benefits of a whole food plant-based diet to your patients? Explore our tips below.
Tips for encouraging healthy eating in your patients
Plantify your favourites: Swap unhealthy ingredients for nourishing plant alternatives.
Focus on the foods you add, not the ones you remove.
Focus on low-calorie density foods: Switch dried fruits to fresh berries.
Out of sight, out of mind: Keep ultra-processed foods out of your fridge or pantry.
Bake or air-fry instead of using oil. Oil is the most calorie-dense food.
Be mindful of liquid calories: Fruit juices and smoothies are easy to overconsume.
Additional Information:
-
Dr Miriam Sonntag is the Medical Content Executive of the online learning platform, PAN Academy. Having worked in basic research, she knows how to decipher complex information. Working now at PAN, she scans and pours over scientific papers and books. She breaks down the latest nutritional research into actionable advice for everyday life. She is committed to sharing the bigger picture of why it is good to put more plants on your plate.
-
World Obesity Federation, 2022. World Obesity Atlas 2022. Available from: https://www.worldobesity.org/resources/resource-library/world-obesity-atlas-2022
National Institute for Health and Care Excellence, 2023. Obesity: identification, assessment and management. Available from: https://www.nice.org.uk/guidance/cg189/chapter/Recommendations#identifying-and-assessing-overweight-obesity-and-central-adiposity
Thomas et al., 2012. Excess body fat in obese and normal-weight subjects. Available from: https://doi.org/10.1017/s0954422412000054
Kahn et al., 2019. Altered adipose tissue and adipocyte function in the pathogenesis of metabolic syndrome. Available from: https://doi.org/10.1172%2FJCI129187
Blüher, 2020. Metabolically Healthy Obesity. Available from: https://doi.org/10.1210/endrev/bnaa004
Lin et al., 2017. The prevalence, metabolic risk and effects of lifestyle intervention for metabolically healthy obesity: a systematic review and meta-analysis: A PRISMA-compliant article. Available from: https://doi.org/10.1097/md.0000000000008838
Ghaben & Scherer, 2019. Adipogenesis and metabolic health. Available from: https://doi.org/10.1038/s41580-018-0093-z
Marcelin et al., 2019. Deciphering the cellular interplays underlying obesity-induced adipose tissue fibrosis. Available from: https://doi.org/10.1172/jci129192
World Health Organization, 2023. Health service delivery framework for prevention and management of obesity. Available from: https://www.who.int/publications-detail-redirect/9789240073234
Guyenet, 2017. The Hungry Brain. Available from: https://us.macmillan.com/books/9781250081230/thehungrybrain
Pontzer, 2022. Burn The Misunderstood Science of Metabolism. Available from: https://www.penguin.com.au/books/burn-9780141990170
Hall et al., 2019. Ultra-Processed Diets Cause Excess Calorie Intake and Weight Gain: An Inpatient Randomized Controlled Trial of Ad Libitum Food Intake. Available from: https://doi.org/10.1016/j.cmet.2019.05.008
Wright et al., 2017. The BROAD study: A randomised controlled trial using a whole food plant-based diet in the community for obesity, ischaemic heart disease or diabetes. Available from: https://doi.org/10.1038/nutd.2017.3
Eichelmann et al., 2016. Effect of plant-based diets on obesity-related inflammatory profiles: a systematic review and meta-analysis of intervention trials. Available from: https://doi.org/10.1111/obr.12439
Duncan et al., 1983. The effects of high and low energy density diets on satiety, energy intake, and eating time of obese and nonobese subjects. Available from: https://ajcn.nutrition.org/article/S0002-9165(23)15614-0/fulltext
de Graaf & Kok, 2010. Slow food, fast food and the control of food intake. Available from: https://doi.org/10.1038/nrendo.2010.41